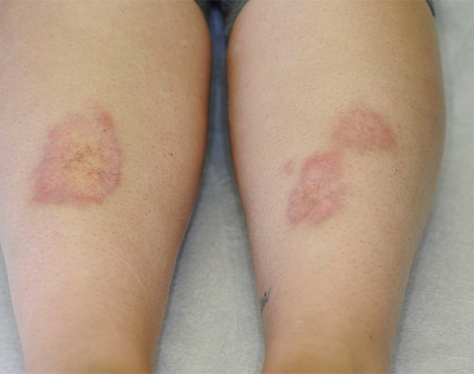
Necrobiosis lipoidica occurs most often in women. It usually presents on shins but may
affect other areas. Reddish yellow plaques enlarge slowly and are generally
asymptomatic, unless they ulcerate. The pathogenesis of the granulomatous inflammation
is uncertain, but many cases are associated with diabetes (necrobiosis lipoidica
diabeticorum). It can precede the diagnosis of diabetes in up to 14% of patients.
Necrobiosis lipoidica shares some features with granuloma annulare, another
granulomatous condition, but one that is rarely associated with diabetes.

What should I look for?
• Oval, well-demarcated papules or plaques, usually on the shin (may be bilateral), that
expand slowly and may coalesce.
• Reddish brown plaques that are smooth, shiny, and telangiectatic.
• The border is erythematous and may be scalloped in outline.
• In older plaques, the reddish centre is more yellow and may be atrophic, revealing
deeper subcutaneous vessels.
• Plaques may ulcerate, but surrounding intact skin generally has some features of
necrobiosis lipoidica.
• Some patients also have granuloma annulare.
What should I do?
• If necessary, take a deep elliptical biopsy to confirm the diagnosis, but the wound may
not heal. The histological features, which overlap with those of granuloma annulare,
include extensive dermal necrobiosis (alteration of collagen bundles) outlined by
histiocytes and giant cells.
• Avoid trauma—use protective shin pads.
• Treatment options include topical and intralesional corticosteroids, and topical 0.1%
tacrolimus, but response is variable.
• Topical corticosteroids, pentoxifylline, nicotinamide with minocycline, and ciclosporin
have been advocated for ulcerated necrobiosis lipoidica.