
Syphilis (the ‘Great pox’), a chronic infectious disease caused by Treponema
pallidum, is increasing in incidence and is a great mimic. The skin is involved at all
stages. patients may not be aware of the 1° lesion. Atypical presentations may be a
sign of HIV/AIDS. Syphilis may be transmitted to the fetus.
What should I look for?
1° syphilis:
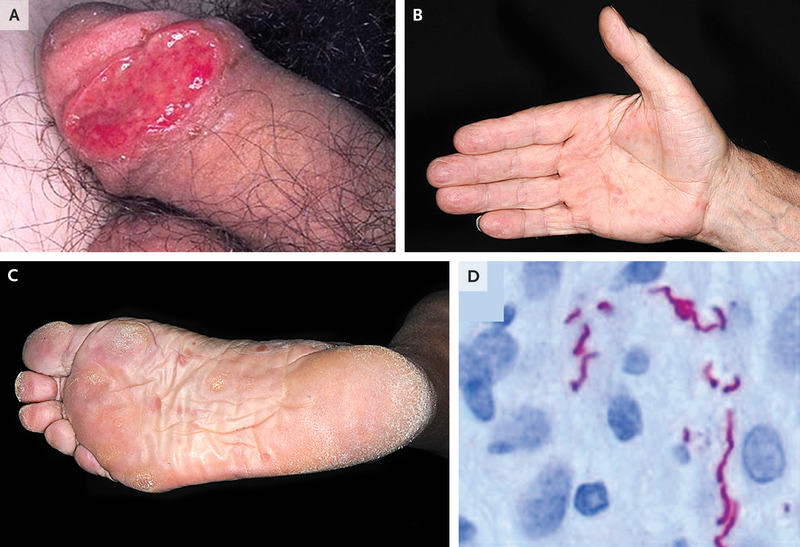
• A solitary, painless, well-demarcated, firm ulcer (chancre), ~1cm in diameter, about
3 weeks after sexual contact. The site of presentation (genitalia, anal, oral, face)
depends on the contact.
• Regional lymphadenopathy.
• A depressed atrophic scar when healed (in around 8 weeks).
2° syphilis:
Presents 1–6 months after 1° infection. Rash settles in 1–3 months.
• Non-itchy symmetrical rash on the face and trunk.
• Initially smooth red macules, then scaly copper-red papules. Scale develops later,
and the rash may resemble psoriasis or cutaneous LE.
• Keratotic papules on the palms and soles.
• Scaly papules on the glans penis or shaft of the penis.
• Macerated hypertrophic flat-topped papules (condylomata lata) in moist
skinfolds—perianal, inframammary, and vulva.
• ‘Split papules’ at the angle of the mouth.
• Patchy moth-eaten hair loss, loss of eyebrows and eyelashes.
• Mucous membranes: greyish white oval patches and erosion on the palate, buccal or
labial mucosa, tongue (‘snail track ulcers’).
• Headache, low-grade fever, lymphadenopathy, and arthralgia.
• Lues maligna (rare): papulopustular rash that rapidly evolves into well-demarcated
crusted ulcers. Seen with co-morbidities causing immunosuppression, e.g. HIV,
chronic alcoholism.
Late (tertiary) syphilis:
May develop years after untreated 1° infection. presentations include neurosyphilis
(tabes dorsalis, general paralysis) and cardiovascular syph- ilis (aortitis) and
gummata. Gummata, painless rubbery nodules that ul- cerate and scar, mainly involve
the skin and bones.

What should I do?
• 1° syphilis: spirochaetes can be isolated from the chancre. Treponemal tests (TTs):
anti-treponemal IgM detected 2 weeks after infection, IgG detected by week 4/5.
Non-treponemal tests (NTTs) react in about 21 days.
• 2° and late syphilis: skin biopsy may be helpful. Serology positive.
• Discuss investigation with a dermatologist or genitourinary physician.
• If diagnosis confirmed, refer the patient to genitourinary medicine for screening for
other STDs, treatment, and contact tracing.