Overview
Postherpetic neuralgia (post-hur-PET-ik noo-RAL-juh) is the most common complication of shingles. The condition affects nerve fibers and skin, causing burning pain that lasts long after the rash and blisters of shingles disappear.
The chickenpox (herpes zoster) virus causes shingles. The risk of postherpetic neuralgia increases with age, primarily affecting people older than 60. There’s no cure, but treatments can ease symptoms. For most people, postherpetic neuralgia improves over time.
Symptoms
The signs and symptoms of postherpetic neuralgia are generally limited to the area of your skin where the shingles outbreak first occurred — most commonly in a band around your trunk, usually on one side of your body.
Signs and symptoms might include:
- Pain that lasts three months or longerafter the shingles rash has healed. The associated pain has been described as burning, sharp and jabbing, or deep and aching.
- Sensitivity to light touch.People with the condition often can’t bear even the touch of clothing on the affected skin (allodynia).
- Itching and numbness.Less commonly, postherpetic neuralgia can produce an itchy feeling or numbness.
When to see a doctor
See a doctor at the first sign of shingles. Often the pain starts before you notice a rash. Your risk of developing postherpetic neuralgia is lessened if you begin taking antiviral medications within 72 hours of developing the shingles rash.
 Causes
Causes
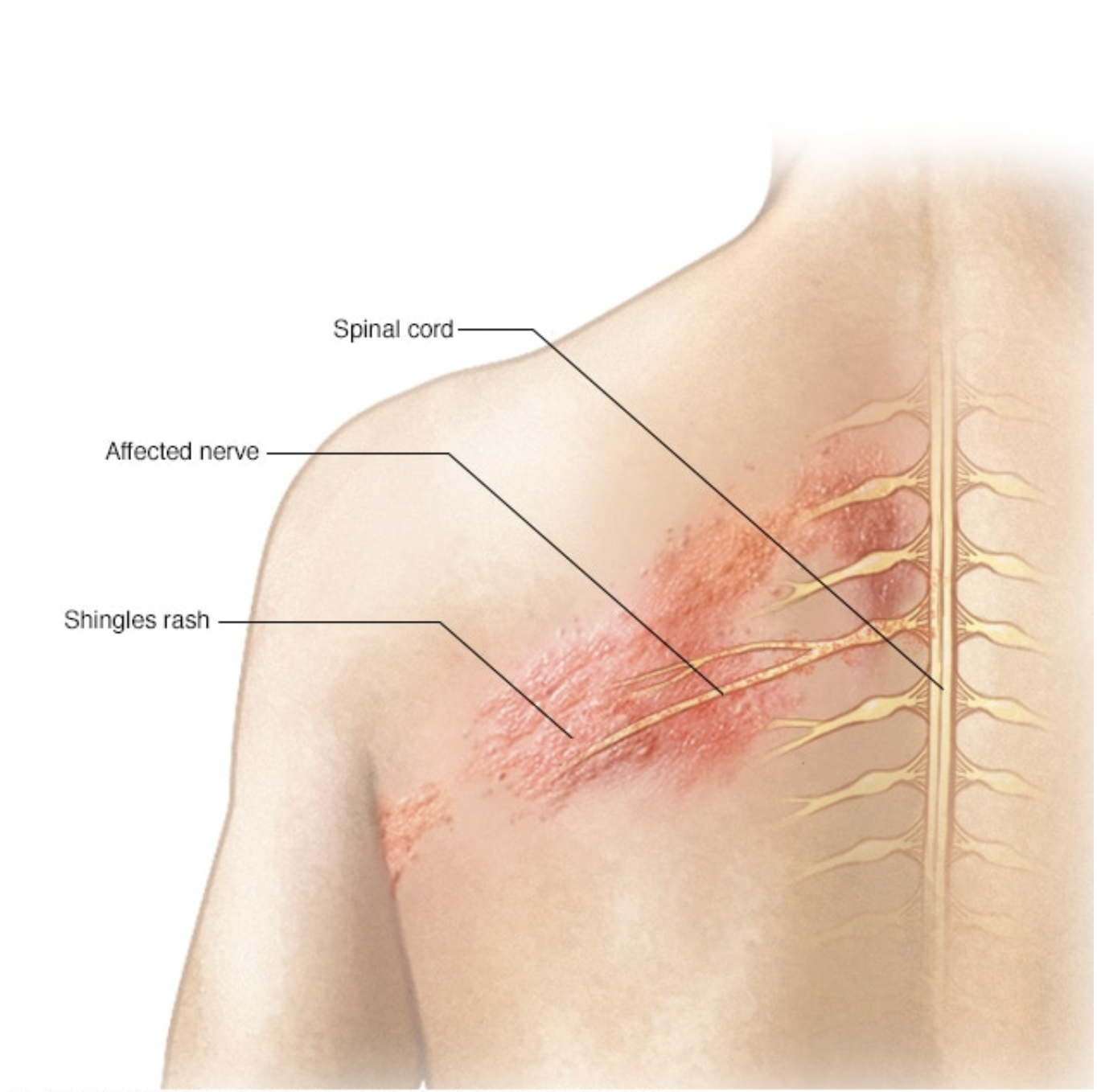
Shingles affects the nerves
Once you’ve had chickenpox, the virus remains in your body for the rest of your life. As you age or if your immune system is suppressed, such as from medications or chemotherapy, the virus can reactivate, causing shingles.
Postherpetic neuralgia occurs if your nerve fibers are damaged during an outbreak of shingles. Damaged fibers can’t send messages from your skin to your brain as they normally do. Instead, the messages become confused and exaggerated, causing chronic, often excruciating pain that can last months — or even years.
Risk factors
When you have shingles, you might be at greater risk of developing postherpetic neuralgia as a result of:
- You’re older than 50.
- Severity of shingles.You had a severe rash and severe pain.
- Other illness.You have a chronic disease, such as diabetes.
- Shingles location.You had shingles on your face or torso.
- Your shingles antiviral treatmentwas delayed for more than 72 hours after your rash appeared.
Complications
Depending on how long postherpetic neuralgia lasts and how painful it is, people with the condition can develop other symptoms that are common with chronic pain such as:
- Depression
- Fatigue
- Difficulty sleeping
- Lack of appetite
- Difficulty concentrating
Prevention
The Centers for Disease Control and Prevention (CDC) recommends that adults 50 and older get a Shingrix vaccine to prevent shingles, even if they’ve had shingles or the older vaccine Zostavax. Shingrix is given in two doses, two to six months apart.
The CDC says two doses of Shingrix is more than 90 percent effective in preventing shingles and postherpetic neuralgia. Shingrix is preferred over Zostavax. The effectiveness may be sustained for a longer period of time than Zostavax. Zostavax may still be used sometimes for healthy adults age 60 and older who aren’t allergic to Zostavax and who don’t take immune-suppressing medications.
Diagnosis
Your doctor will examine your skin, possibly touching it in places to determine the borders of the affected area.
In most cases, no tests are necessary.
Treatment
No single treatment relieves postherpetic neuralgia for everyone. It often takes a combination of treatments to reduce the pain.
Lidocaine skin patches
These are small, bandage-like patches that contain the topical pain-relieving medication lidocaine. These patches can be cut to fit only the affected area. You apply the patches, available by prescription or over-the-counter at a slightly lower dosage, directly to painful skin to deliver temporary relief.
Capsaicin skin patch
A high concentration of an extract of chili peppers (capsaicin) is available as a skin patch (Qutenza) to relieve pain. Available only in your doctor’s office, the patch is applied by trained personnel after using a numbing medication on the affected area.
The process takes at least two hours because you need to be monitored after the high-concentration patch is applied, but a single application decreases pain for some people for up to three months. If it works, the application can be repeated every three months.
Anticonvulsants
Certain anti-seizure medications, including gabapentin (Gralise, Horizant, Neurontin) and pregabalin (Lyrica), can lessen the pain of postherpetic neuralgia. These medications stabilize abnormal electrical activity in your nervous system caused by injured nerves. Side effects include drowsiness, unclear thinking, unsteadiness and swelling in the feet.
Antidepressants
Certain antidepressants — such as nortriptyline (Pamelor), amitriptyline, duloxetine (Cymbalta) and venlafaxine (Effexor XR) — affect key brain chemicals that play a role in both depression and how your body interprets pain. Doctors often prescribe antidepressants for postherpetic neuralgia in smaller doses than they do for depression alone.
Common side effects of these medications include drowsiness, dry mouth, lightheadedness and weight gain.
Opioid painkillers
Some people might need prescription-strength pain medications containing tramadol (Ultram, Conzip), oxycodone (Percocet, Roxicet) or morphine. Opioids can cause mild dizziness, drowsiness, confusion and constipation.
However, recent CDC guidelines urge doctors to consider treatments other than opioids for pain that isn’t cancer-related, such as the pain of postherpetic neuralgia. This is based on increasing recognition of the risk of addiction and death in some people using opioids.
If prescribed, opioids need to be monitored closely, used at the lowest possible dose and considered only in situations where safer medications have failed.
Opioid medication can impair your ability to drive and should not be combined with alcohol or other drugs.
Steroid injections
Steroids are sometimes injected into the spine (intrathecal or epidural) for postherpetic neuralgia. However, evidence of effectiveness is inconsistent. A low risk of serious side effects, including meningitis, has been associated with their use.
Lifestyle and home remedies
The following over-the-counter medications may ease the pain of postherpetic neuralgia:
- Capsaicin cream, made from the seeds of hot chili peppers, might relieve pain from postherpetic neuralgia. Capsaicin (Capzasin-P, Zostrix, others) can cause a burning sensation and irritate your skin, but these side effects usually disappear over time.
Because capsaicin cream can irritate your skin, avoid getting it on unaffected parts of your body. Follow instructions, including wearing gloves for application and washing your hands thoroughly after applying.
- Topical analgesics and anesthetics.Aspirin crushed and mixed into an absorbing cream or nonprescription-strength lidocaine cream might reduce skin hypersensitivity.
Preparing for your appointment
You might start by seeing your family doctor. He or she may refer you to a nerve specialist (neurologist) or a doctor who specializes in treating chronic pain.
Here’s information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there’s anything you need to do in advance, such as fasting before a specific test. Make a list of:
- Your symptoms,including any that seem unrelated to the reason for your appointment, and when they began
- Key personal information,including major stresses, recent life changes and family medical history
- All medications, vitamins or other supplementsyou take, including doses
- Questions to askyour doctor
Take a family member or friend along, if possible, to help you remember the information you’re given.
For postherpetic neuralgia, questions to ask your doctor include:
- What’s likely causing my symptoms?
- What else could cause my symptoms?
- What tests do I need?
- Is my condition likely temporary or chronic?
- What’s the best course of action?
- What are the alternatives to the primary approach you’re suggesting?
- I have other health conditions. How can I best manage them together?
- Are there restrictions I need to follow?
- Should I see a specialist?
- Are there brochures or other printed material I can have? What websites do you recommend?
Don’t hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you several questions, such as:
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- Have you had chickenpox? When?
- Have you had a shingles vaccine?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?